Key Points
A breast pump helps you remove breast milk from your breasts.
Pumping may be helpful if you’ll be away from your baby or if someone else, like your partner, is feeding your baby.
You can use a manual pump or a pump that uses batteries or electricity. Your health insurance may help pay for your pump.
You can store pumped milk in a refrigerator or freezer for later use.
Do all breastfeeding moms use a breast pump?
No. But if there are times you’ll be away from your baby, like if you’re going back to work or school, you may need a breast pump. A breast pump helps you remove breast milk from your breasts. You can use the milk at a later time to feed your baby. Breast milk that you pump from your breasts is called expressed milk.
Breast pumps can help you in lots of ways:
- If you go back to work or school, you still can feed your baby breast milk.
- Your partner or another caregiver can feed your baby breast milk.
- Pumping helps keep your breast milk from building up in your breasts. This helps prevent discomfort and infection.
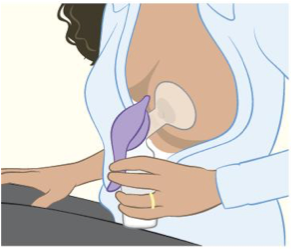
How do breast pumps work?
All pumps have a shield that covers your breast and a container that collects breast milk. If you’re not sure what kind of pump is best for you, ask your lactation consultant. This is a person who has special training to help women breastfeed. Check with your health insurance company to see if it helps pay for a pump.
You may not know how often you’ll need to pump until you have your baby. So you may want to wait until after your baby is born to get one.
There are two kinds of breast pumps:
Manual pump. This is a pump that you work by hand. You can use a manual pump anywhere because it doesn’t need electricity.
This kind of pump is good if you don’t need to pump very often or if you don’t need a lot of milk at one time.
Powered pump. This pump uses batteries or electricity. It has a motor to pump your breasts.

You can use a single pump that works on one breast at a time. Or you can use a double pump that works on both breasts at the same time. If you’re going back to school or work, you may like double pumps because they’re faster than single pumps.
Can you rent or share a breast pump?
Breast pumps are single use (made for just one user) or multiple use (made for more than one user). Multiple-use pumps are made so that any part that touches breast milk (like the shield, tubes and the container) is new for each user.
It’s OK to rent or share a breast pump only if:
- It’s multiple use.
AND
- It comes from an authorized provider, like a hospital, medical supply store or a lactation consultant.
Sharing breast pumps can be dangerous. If the pump and all its parts aren’t fully cleaned, it can spread infection and be dangerous for you and your baby. Here’s how to keep your pump and your breast milk safe:
- Don’t rent or share a manual breast pump. Manual breast pumps are single use only.
- Don’t rent or share a single-use powered pump. Only rent or share a powered pump that’s multiple use.
- Only share or rent a multiple-use pump from an authorized provider. These providers can help you choose the right pump and give you new, clean equipment to use with the pump.
- Don’t share any pump with your family or friends. Only share a pump that comes with clean equipment from an authorized provider.
Sharing a breast pump may affect its warranty. So if you share the pump and have problems with it (like it doesn’t work), you may not be able to get help from the company.
When can you start pumping?
Talk to your health care provider about when you can start pumping breast milk. You may want to start pumping soon after your baby is born. This can help build up your milk supply, and you can freeze the expressed breast milk to use later. Your milk supply is the amount of breast milk you make for each feeding. Pumping your breasts after your baby breastfeeds can help you increase your milk supply.
Wait until your baby is breastfeeding well before you start feeding him pumped breast milk from a bottle. Starting your baby on a bottle (or giving him a pacifier) too early can cause nipple confusion. This is when your baby has trouble latching on and sucking after being given a bottle or pacifier. Your baby forgets how to latch on to your breast, so he doesn’t feed well or doesn’t want to breastfeed.
If you’re going back to work or school:
- Start pumping at least 2 weeks before you go back.
- Try to pump as often as your baby usually feeds. This may be every 3 to 4 hours for about 15 minutes each time.
- Find a private place to pump. If your workplace has more than 50 employees, your employer is required by law to give you time and space (that’s not a bathroom) for pumping. Talk to your boss before you go back to work so he knows what you need.
Can you store breast milk?
Yes. You need a few supplies to keep breast milk fresh and safe for your baby after pumping:
- Bottles or bags. These are made just to store pumped breast milk. The bags are plastic, and the bottles are plastic or glass. You can buy them at most grocery stores, drug stores or baby stores.
- A cooler. Use a small cooler to keep your pumped milk cold until you get it home. You may need a cooler if you don’t have a refrigerator at your work or school. Your breast pump may come with a cooler.
Here’s how to store pumped breast milk:
- Wash your hands and the container (bottle or bag).
- Write the date on the container. If your baby stays with a child care provider, write your baby’s name on the container, too.
- Put just the amount of milk your baby needs for each feeding in each container. This is about 2 to 4 ounces of breast milk.
- Store the container in the refrigerator or freezer.
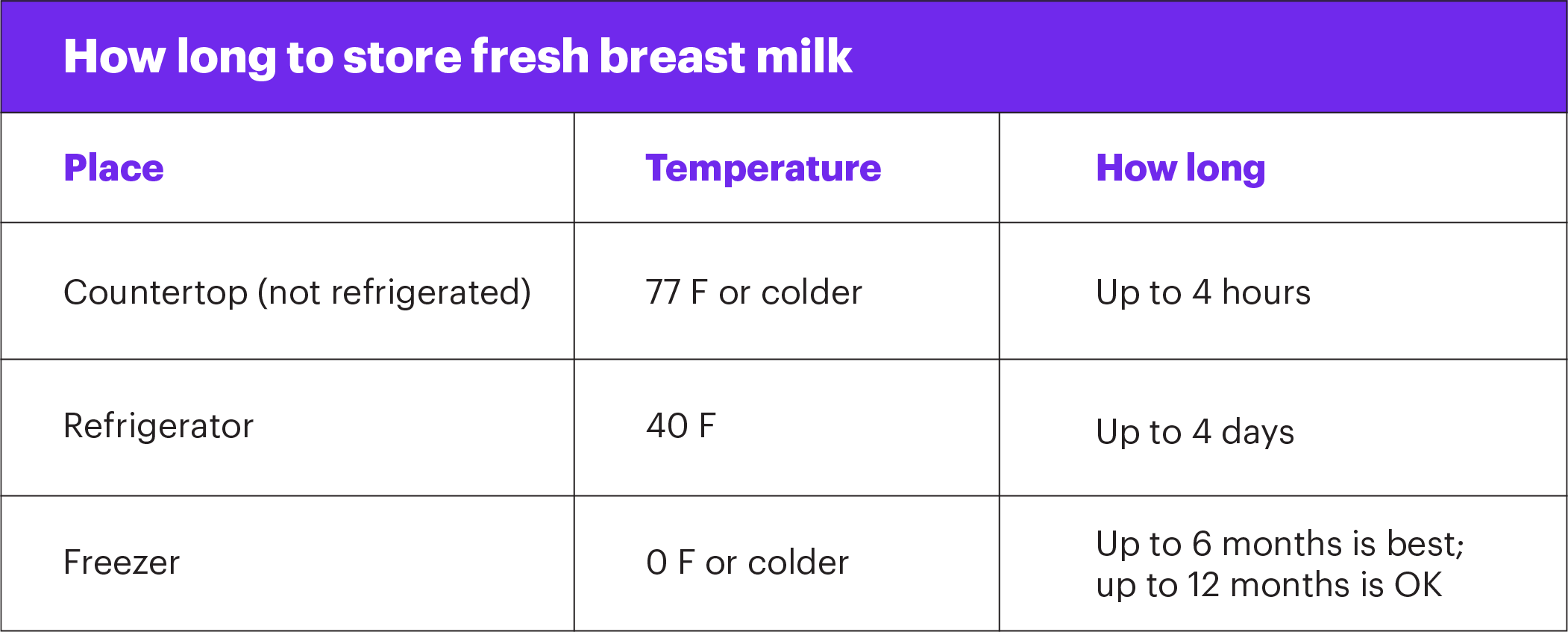
How long can you store breast milk?
Use these guidelines for storing breast milk.
How do you thaw and warm breast milk once you’re ready to use it?
To thaw frozen breast milk:
- Make sure the container is sealed tight.
- Put the container under running cold water.
- Pour the amount of thawed milk you need for your baby into a bottle for feeding.
- Use the thawed milk within 24 hours. Don’t refreeze breast milk after it’s been thawed.
To warm thawed or refrigerated milk:
- Put the container under running hot water or in a bowl of warm water.
- Pour the amount of milk you need for your baby into a bottle for feeding.
- Put a drop or two of milk on the back of your hand to test the temperature. If it’s too hot, let it cool.
- Never heat breast milk in the microwave. It kills nutrients in the milk and can burn your baby’s mouth.
More information
American Academy of Pediatrics
International Lactation Consultant Association
womenshealth.gov/breastfeeding
Last reviewed: June, 2019